Deep Vein Thrombosis (DVT) often develops quietly, without dramatic symptoms. But the danger it presents is anything but silent. When a blood clot forms in the deep veins typically in the legs. It can break loose, travel through the bloodstream, and block a vessel in the lungs. This potentially life-threatening complication is called a Pulmonary Embolism (PE).
This guide is here to help you understand the connection between DVT and PE, recognize early signs, and take proactive steps for prevention and treatment. Early awareness could save your life or someone else’s.
What is Deep Vein Thrombosis?
Deep Vein Thrombosis is a condition in which a blood clot (thrombus) forms in one of the deep veins of the body, usually in the lower leg, thigh, or pelvis. The clot can partially or completely block blood flow, leading to pain and swelling. However, many people don’t notice symptoms at all.
What is a Pulmonary Embolism?
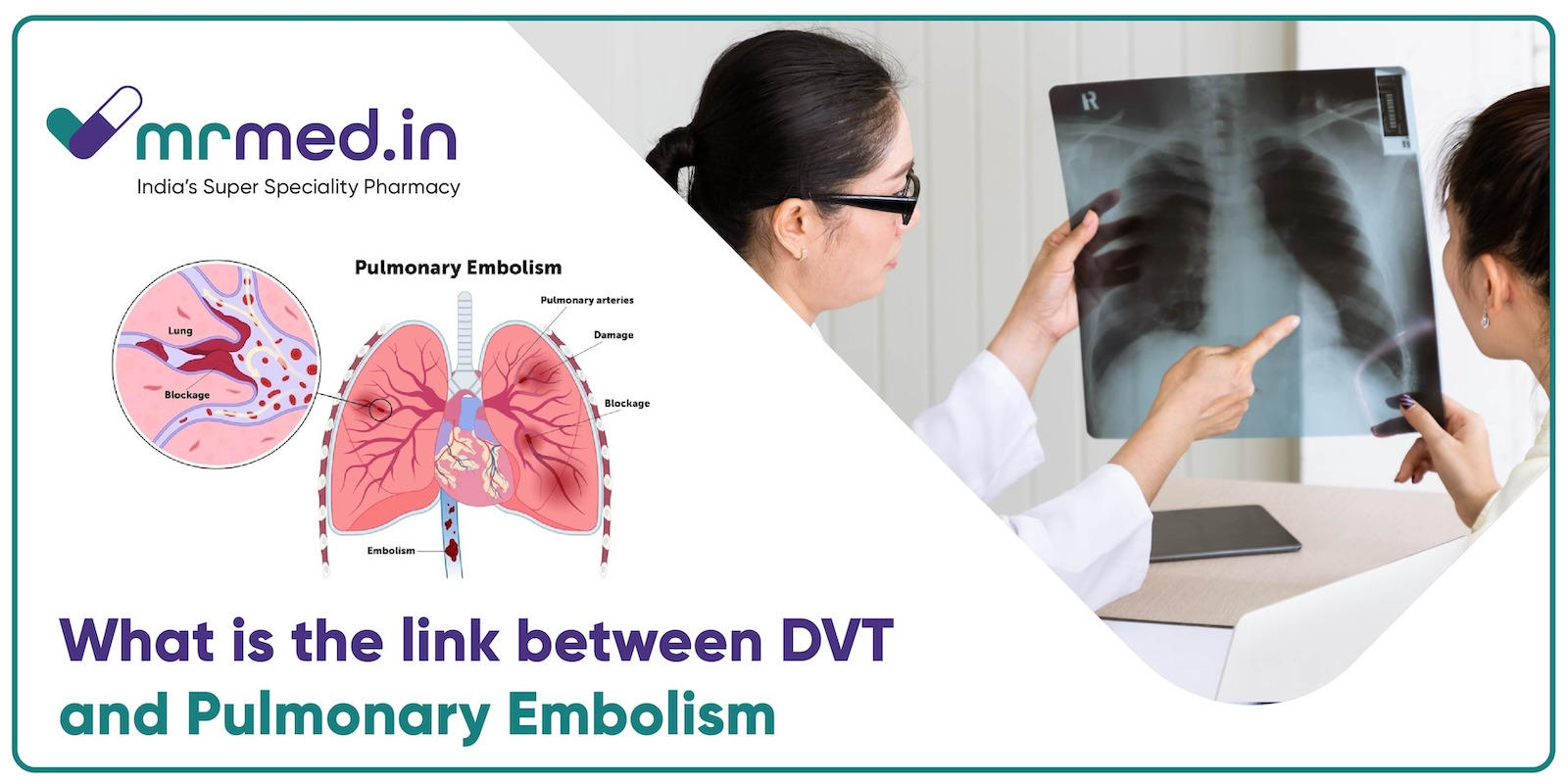
A Pulmonary Embolism (PE) happens when a part of a DVT clot breaks free, travels through the bloodstream, and becomes lodged in the lungs. This blockage can reduce or completely stop blood flow to part of the lung, preventing oxygen from reaching the body. In severe cases, PE can cause sudden death.
How DVT Leads to Pulmonary Embolism?
The clot that starts in a leg vein during DVT can dislodge and enter the circulatory system. It travels up through larger veins, passes through the right side of the heart, and gets stuck in the pulmonary arteries, creating a pulmonary embolism.
If the clot is large, it can block major lung arteries, making it extremely hard for the heart to pump blood through the lungs. This can cause chest pain, sudden shortness of breath, low oxygen levels, and in worst cases heart failure or death.
What are the Symptoms of DVT and PE?
Symptoms of DVT:
- Swelling, usually in one leg
- Pain or tenderness not caused by injury
- Warmth or redness over the affected area
- A tight feeling in the calf
Symptoms of PE:
- Sudden shortness of breath
- Chest pain that may get worse with deep breathing or coughing
- Coughing up blood (hemoptysis)
- Rapid heartbeat or breathing
- Lightheadedness, fainting, or dizziness
Who is at Risk?
There are several things that can make someone more likely to get Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE), which is a serious thing that can happen because of DVT. If a person is still for a long time, like when in bed, during long trips, or sitting a lot at work, blood flows slower in their legs, which can cause clots to form. Surgery can be risky too, especially on the hips, legs, or belly, since it makes it hard to move and can hurt tissues. Injuries, cancer, cancer treatments, and situations such as being pregnant or having given birth recently can make blood clot easier. Lifestyle choices like smoking and being overweight raise the risk even more. Also, if a person or their family has had blood clots before, that adds to the risk. Understanding these risks helps prevent DVT and PE, especially if someone has more than one risk factor.
Diagnosis: How Are DVT and PE Detected?
DVT Detection
- Ultrasound of the leg to detect blood flow blockages
- D-dimer blood test to detect clot-related proteins
- Venography, an X-ray of veins with dye (rarely used)
PE Detection
- CT Pulmonary Angiography (CTPA): A scan that visualizes clots in the lungs
- V/Q scan: Which checks airflow and blood flow in the lungs
- D-dimer test: Often used to rule out clots
Treatments That Can Save Lives
1. Anticoagulants (Blood Thinners): These are the first line of defense. Medications like warfarin, apixaban, or rivaroxaban help prevent new clots and stop existing ones from growing.
2. Heparin Injections: Often used in hospitals, Heparin is a fast-acting anticoagulant given through injections or IV. It helps stabilize patients with DVT or PE and is sometimes used before switching to oral medications.
3. Thrombolytics (Clot-busting medications): For severe PE, especially when life-threatening, Medications like Alteplase (brand name Actilyse) can be used to break up clots quickly. These medications carry bleeding risks and are used in critical situations.
4. Filters and Surgery: In rare cases, a vena cava filter may be placed in a large vein to catch clots before they reach the lungs. Surgery to remove a clot (embolectomy) is also an option in extreme cases.
Preventions of Pulmonary Embolism
- Move regularly: Stand, stretch, or walk every couple of hours, especially on long trips or after surgery.
- Stay hydrated: Dehydration thickens the blood, raising clot risk.
- Wear compression stockings: Especially after surgery or during long flights.
- Manage chronic conditions: Control diabetes, high blood pressure, and other risk factors.
- Avoid smoking and maintain a healthy weight.
Key Takeaways
Deep Vein Thrombosis is more than just a clot in your leg it can be the beginning of a dangerous chain reaction. If that clot moves to the lungs, it can cause a Pulmonary Embolism, a medical emergency that can turn deadly in minutes. Understanding the symptoms, getting early treatment, and following prevention strategies, anticoagulants, and staying active can make all the difference. If you or someone you love has symptoms of DVT or PE, don’t wait. Seek immediate medical care.